Radiation technologies
Contemporary radiation technologies for an effective therapy of cancer tumours
The Radiotherapy Pasing is equipped with two most advanced linear accelerators from Varian Medical Systems. With these irradiation devices we can carry out all common therapy procedures. One of these devices - the TrueBeam - is Germany's first device in this high-end series with iterative CBCT - for even greater precision, even better tumor control, and even fewer side effects.
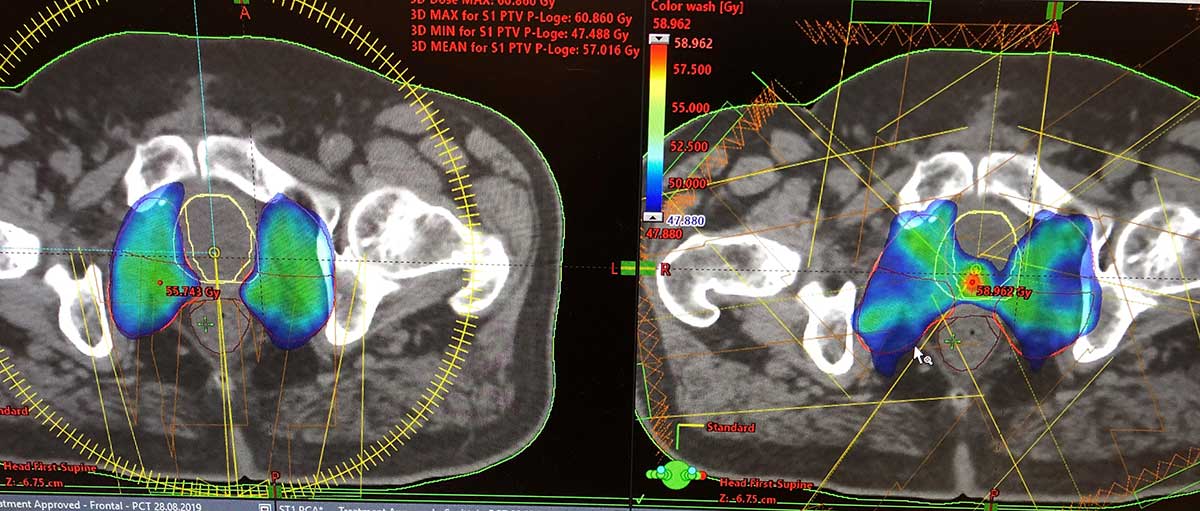
Prostate patient: Rapid Arc (left) vs. IMRT (right)
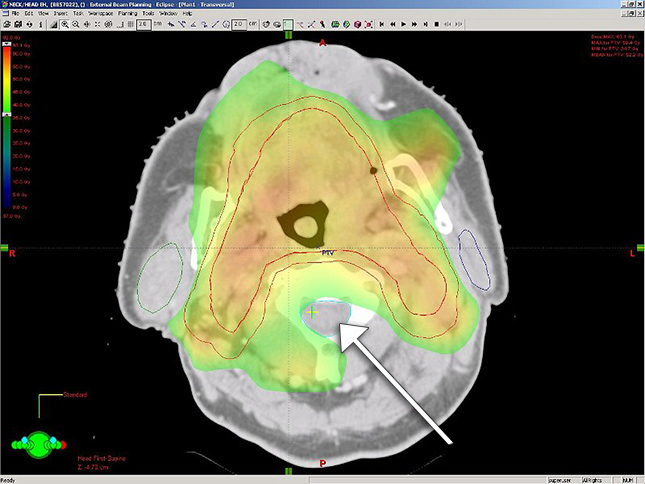
RapidArc for ENT patients
RapidArc is the irradiation technique with which it is best possible to distinguish between healthy tissue - which should be spared as much as possible - and tumor tissue in certain regions, for example the prostate or the ENT area.
While the irradiation device rotates around the patient and the slats forming the beam are also moving permanently, a treatment beam is generated. Through these double movements during the beam phase, we can precisely regulate the strength of the therapy beam in the tissue.
On the one hand, this ensures that the entire tumor area receives exactly the dose that we specify. On the other hand, the directly adjacent healthy tissue is even better protected, as the dose in this area very quickly becomes very low. This leads, among other things, to the fact that the dose in the tumor can be increased - in many cases this significantly increases the chances of the tumor tissue being completely destroyed while at the same time the side effects become fewer. In addition, this technique significantly reduces treatment times, so that the individual radiation session is much shorter than with conventional radiation techniques.
If this technology is combined, for example in the prostate, with Goldmarker tracking, tumors and organs that are moving can be irradiated with extreme precision.

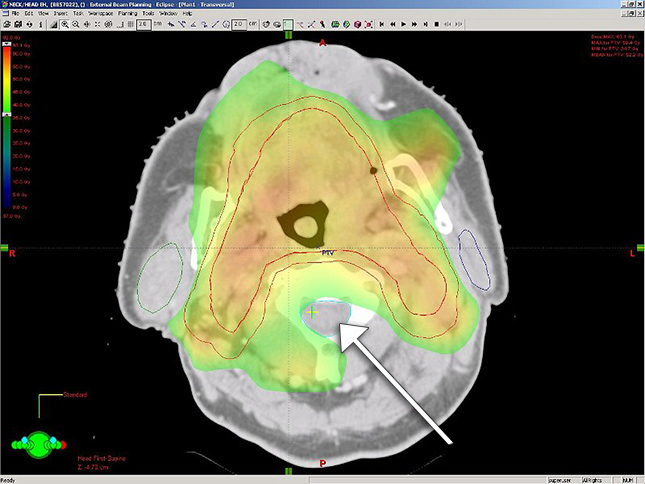
Conventional CBCT (upper row) vs. Iterative CBCT (lower row): the newly developed software calculates image disturbances and thus enables a very precise differentiation between tumor and normal tissue
With the new Varian TrueBeam we have installed the most modern device in Munich with the first iterative CBCT in Germany (here link to the section "Image Guided Radiotherapy (IGRT) and Goldmarker"). The iterative imaging procedure allows for an even more precise irradiation of the tumor and allows for further protection of healthy tissue. The improved visibility of soft tissues and reduced image disturbances allows highly precise therapy planning and increases the effectiveness on the tumor, which further improves the chances of healing with fewer side effects.
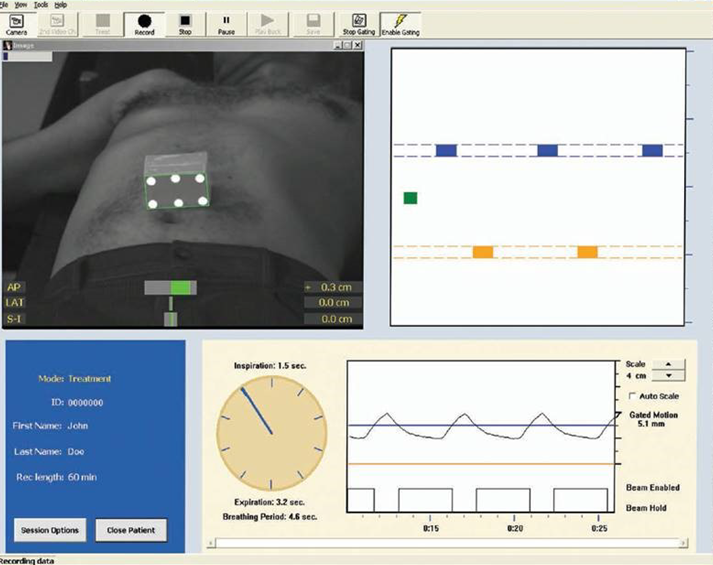
Goldmarker tracking
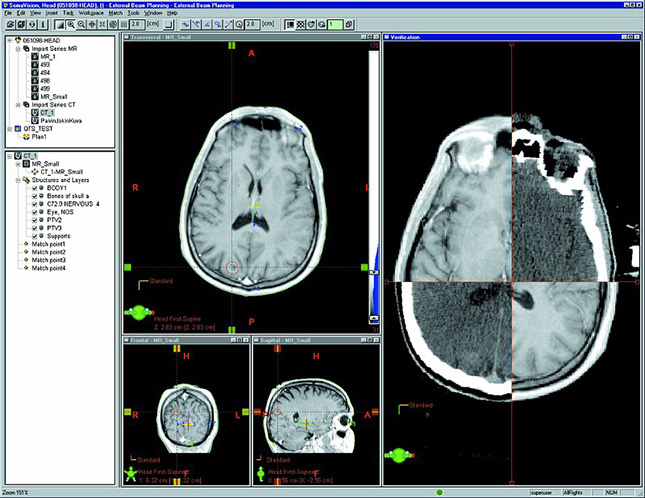
Radiotherapy planning with exact positioning with the aid of precise imaging information.
IGRT is an image-guided radiation therapy. Since the area to be irradiated must of course be hit very precisely by the beam, there are various techniques that can be combined to ensure millimeter-accurate and reproducible irradiation.
On the one hand, this includes the skin markings made with a pen during the planning CT. On the other hand, it also includes x-rays, which are taken at regular intervals during the radiation phase and evaluated immediately.
Using these X-ray images, special image processing programs are then used to ensure that the patient and thus also the region to be irradiated are exactly positioned before the irradiation.
With a computer tomograph (CBCT) integrated into the irradiation device, the tumour and the neighbouring organs in the body can be monitored during the irradiation. Possible movements (e.g. due to breathing during the irradiation of lung tumors) can thus be optimally compensated for by readjusting the therapy beam accordingly. This increases the precision and effectiveness at the tumor while reducing the irradiated tissue and thus the side effects.
In some cases - e.g. when irradiating the prostate - it may be useful to insert small goldmarkers into the target organ or tumor. These so-called gold markers are only a few millimetres in size and are completely harmless; however, in certain cases they ensure that we can determine the irradiated region even better and more precisely in the context of therapy planning and implementation.
Prostate cancer patients in particular benefit from so-called goldmarker tracking, because tumors in these regions move during irradiation. With this method, the small marker pins, which were previously inserted gently into the tumor, can be found independently by the device so that the beam guidance can be readjusted during irradiation. Surrounding tissue is thus spared and a higher dose can be administered in a shorter time.
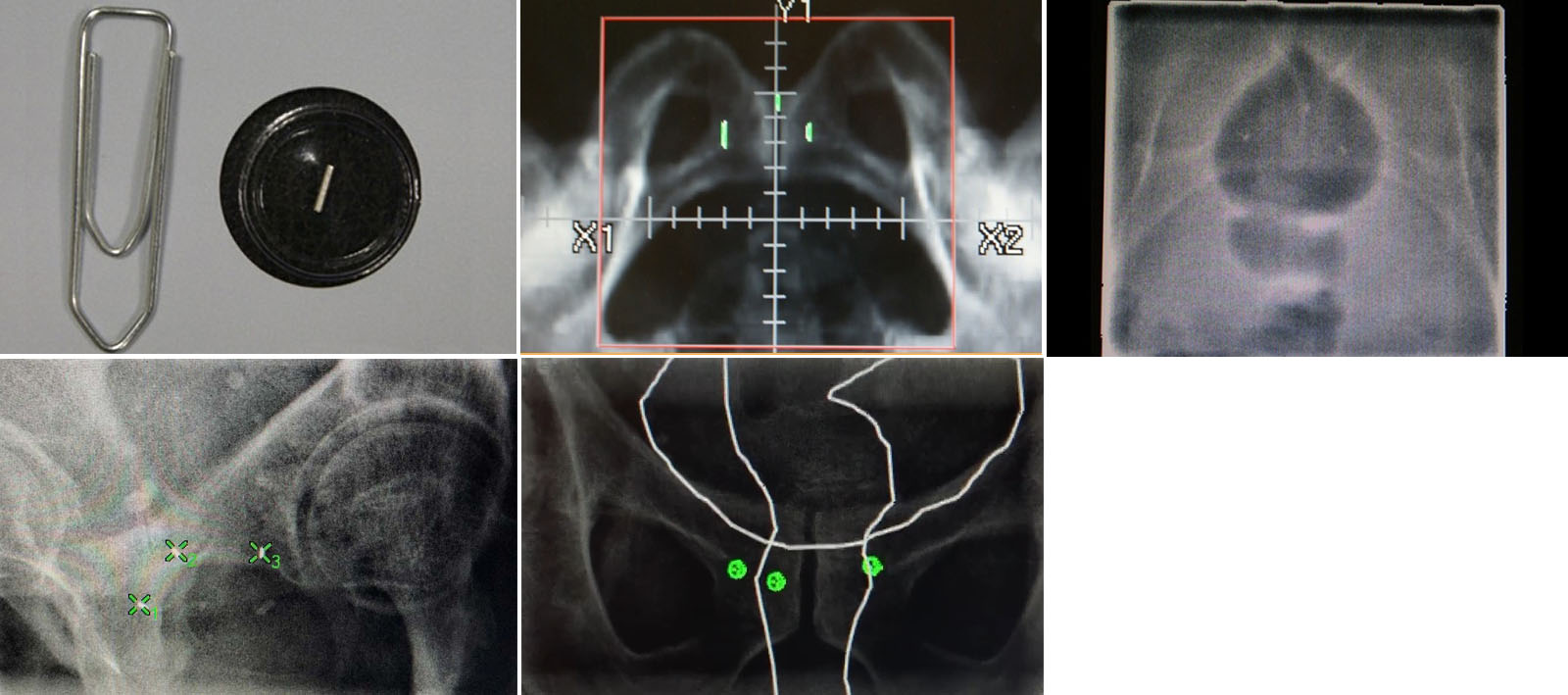
Irradiation of the prostate before and today - optimal protection of the intestine
ENT radiation - optimal protection of the spinal cord
Tissue-friendly and more intensive radiation with rays directed around the curve
This radiation technology is a highly complex development of the previous three-dimensional radiation technology. The use of IMRT is useful in many, but not in all cases.
The main difference to the standard three-dimensional radiation techniques is that the IMRT can be used to irradiate "around the curve", so to speak. This enables optimal radiation or protection of concave or convex structures and is particularly useful for radiation to the prostate or in the ear, nose and throat area.
With this radiation technique it has become possible in many cases to increase the radiation dose in the tumor and at the same time to protect the neighboring organs better - overall, this technique has made radiation therapy even more effective in combating cancer.
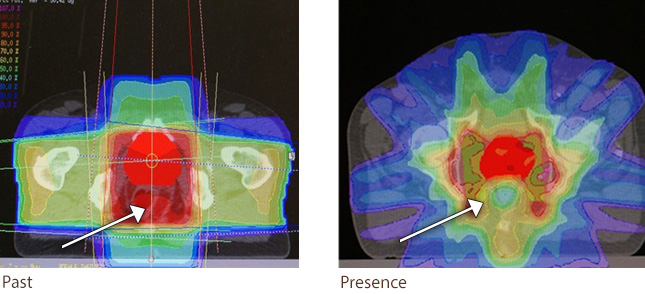
Example of a small-volume, high-dose irradiation of a brain metastasis
Irradiate small tumors precisely and with high doses
In the case of small tumors, it may make sense to use special radiation techniques to optimize the success of the therapy.
Stereotaxy or small-volume high-precision radiation is radiation therapy with higher single doses in one or only a few therapy sessions in which small tumors are irradiated with the highest precision. Since the dose per session is usually significantly higher than that of conventional radiation therapy, it is particularly important here to protect the neighboring structures.
In addition to the special equipment required for the radiation device and the necessary software, special positioning aids for positioning the patient must be used with this technique. This achieves an optimal dose distribution in the tumor with a rapid dose drop in the neighboring area. This ensures that this technique can also be used to safely and effectively irradiate high individual doses. Such a small-volume, high-precision irradiation is suitable, for example, for the following diseases:
- Single or few brain metastases
- Small lung tumors or single or few lung metastases
- Small liver tumors or single or few liver metastases
- Single or few bone and lymph node metastases
- Benign brain tumors
The Bavarian State Chamber of Physicians has given us the certificate for the "special qualification for performing stereotactically guided precision radiation therapy / radiosurgery". We can therefore offer small-volume, high-dose radiation therapy to some of the patients with the above-mentioned diseases.
However, we also work with institutions that specialize exclusively in this type of therapy. If, when looking through the documents, it turns out that the patient benefits more from being treated in such a facility, we organize this together with the colleagues on site. The most important thing is that the patient receives the optimal therapy for him.
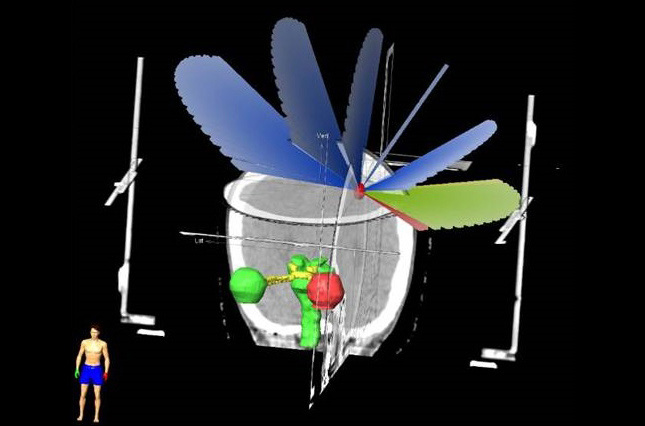
Breath dependent radiation
As a result of breathing, tumours in the lungs, but also the organs in the chest and abdominal area continuously change their position.
This mobility is compensated for by respiratory gating: radiation is only administered during a certain breathing phase (e.g. deep inhalation). The irradiation device detects - monitored by highly qualified MTRAs and the physicians - in which phase of the patient's respiratory movements the therapy beam must be generated.
In this way, optimum protection of the lungs or heart can be achieved.
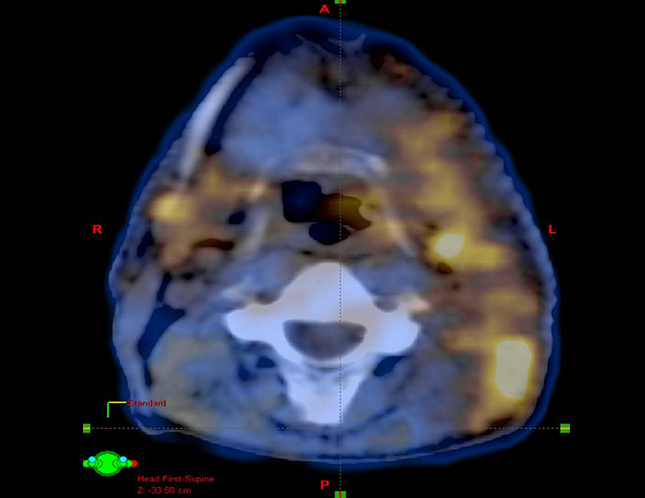
PET-CT fusion: tumor in the ENT area
CT/Bundle tumor information from different image sources
Bundle tumor information from different image sources
Optimal information yield by utilizing all available information
There are very different methods today to make a structure inside the body visible. The palette ranges from the traditional X-ray image to the modern CT imaging (computed tomography) and MRI (nuclear spin) to highly complex functional examinations such as PET-CT (positron emission tomography / computed tomography) or fMRI (functional magnetic resonance imaging), with which the properties can be determined Can make cells and cell systems visible. These different processes mean that a structure can now be recognized and delimited very precisely.
For example, if you examine a tumor using different methods, you can then bundle the information from all the examinations and thus obtain an optimal information yield. This bundling is called image fusion in radiation therapy planning, i.e. the amalgamation of all image information with the aim of optimally displaying the tumor and the structures adjacent to it, in order to then enable equally optimal therapy.
Since we also have specialist expertise in diagnostic radiology and broad knowledge in nuclear medicine procedures, we can use all image information in a highly professional manner for the greatest possible therapeutic success.
Therefore, all available image information is used for the preparation of our therapy plans and is included in the planning accordingly.


